[PRESS RELEASE] Cross-Border Insights into Lao PDR’s Evidence-Informed Health Policy with HTA: First-Ever Study Maps the Way Forward

The Delta variant that was first detected in September 2020 in India led to a major outbreak around April 2021. This variant crowded out others due to its higher transmission rate, and it soon became a concern for the rest of the world before the recent surge, on account of the Omicron variant, eclipsed it.
India’s experience in containing the second wave of the infection offers lessons learned for neighbouring countries in the region and beyond on how to respond to potential future infections.
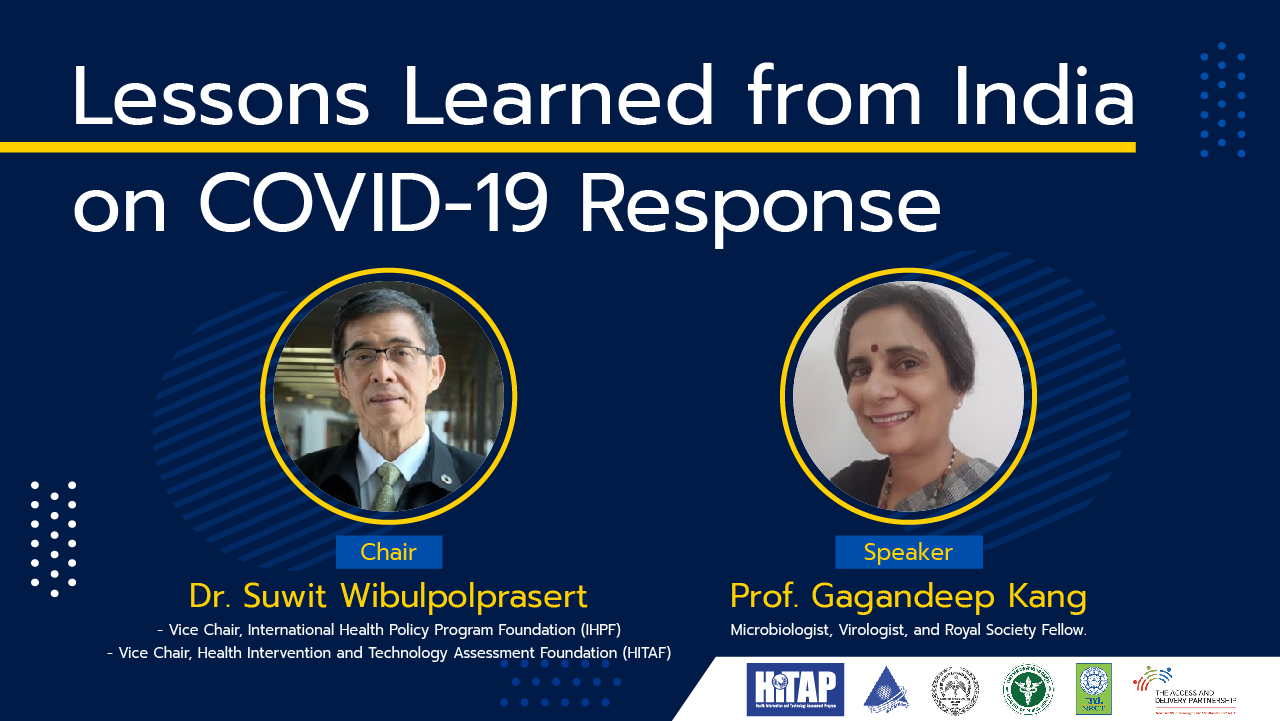
Recognising the importance of knowledge sharing, the Health Intervention and Technology Assessment Program (HITAP) hosted a webinar on October 14, 2021, with Prof. Gagandeep Kang, an eminent scientist and practitioner at the Christian Medical College (CMC) Vellore, and chaired by Dr. Suwit Wibulpolprasert, a senior official at the Ministry of Public Health, Thailand.
In his opening remarks, Dr. Wibulpolprasert highlighted that this has been the greatest pandemic in the last 68 years and people are exploring unchartered territory. Prof. Kang added that given this dynamic environment, countries will need to adapt their responses depending on the evolving situation.
The second COVID-19 wave in India
During the second wave of COVID-19 in India from April to May 2021, there was a dramatic rise in cases, up to 400,000 cases/day. The cumulative case numbers placed India after the US, and in terms of the cumulative death rate, it was the third highest.
The official numbers did not, however, capture the actual conditions since they relied on the testing capacity. Prof. Kang noted that the official data was 10 times lower than the household-level serosurveys. In the case of Bhopal city, the cremation ceremony registrations were 24 times higher compared to the official death reports, which indicated a potential undercounting of deaths due to COVID-19.
Serosurveys detect infection through the presence of sufficient and specific antibodies that indicate previous infections. This approach enables the estimation of infection in an asymptomatic population and can go beyond what is identifiable based on testing capacity.
The serosurveys from India told that infection prevalence was growing from 0.73% to more than 50% and was concentrated in urban slums, in May 2020 to July 2021. The level of infections (50-60%), however, does not translate into herd immunity in the entire population. Given the possibility of reinfection and reopening the country, the susceptible population would not be protected.
How did the government respond to the situation?
The federal government declared the outbreak as a disaster on 14 March 2020 which allowed it to release funds under the National Disaster Management Act 2005. The funds were used, among other things, to provide compensation to families who lost members due to COVID-19. A lockdown also instated, and it attracted strong criticism due to its strict implementation.
Entering the second wave, India was overwhelmed by the number of active cases and the need for medical oxygen, which required a better public health response. Many private and public hospitals were converted into COVID-19 hospitals, increasing the number of facilities such as Intensive Care Units (ICU) beds. There were sufficient facilities and COVID-19 care camps were set-up even for migrants. However, the quality of the facilities varied.
The number of private laboratories involved in mass testing also increased. However, India did not develop a wide testing capacity in collaboration with private laboratories even though they could have played a critical role in supporting the response, although this could have countered the official narrative of low number of cases.
The situation was quite different during the influenza A virus subtype H1N1 (A/H1N1) outbreak, where there was an attempt to involve private laboratories in the testing process, recognising that they had wider public reach.
Testing in India is also relatively inexpensive, compared to global prices: India’s real-time polymerase chain reaction (RT-PCR) price at private laboratories is capped at $22. In Thailand, it is higher and costs approximately $60.
India focused on self-reliance due to a global supply shortage and lockdown conditions, which caused manufacturers and other sectors to ramp diagnosis capacity. This condition caused testing quality and standards for validation to remain an issue. Decision-makers in other countries must acknowledge such situations in their response plans.
Another key lesson for countries is to include the right composition of multidisciplinary experts in the federal and state committees to formulate the policy responses. India’s central committee was established rather slowly and lacked experts in communicable diseases, which delayed the estimation of the trajectory of the virus transmission and other public health actions.
What would India do for the next wave?
It is possible that India may experience another wave, but it might not be as severe or high in caseload as the second wave given the on-going vaccination drive in India. In addition, the seropositivity would likely have increased above 67% positivity after May 2021 as a more recent serosurvey after June in the state of Kerala showed a seropositivity rate of 85% in adults.
This suggests that the remaining susceptible population would be only around 200 – 250 million out of a 1.4 billion population and the new infections would be only flare-up of cases as transmission occurs within families or population groups that are continuing to be susceptible.
This narrative could change with the arrival of a new variant that is able to escape the immune response and transmit easily. However, India has strengthened its genomic surveillance. Other countries like Thailand may or may not face the same situation, and infections will depend on the proportion of the susceptible population and the vaccination rate.
Conclusion
As COVID-19 keeps evolving, learning the valuable lessons from the Indian government’s response during the second outbreak would be relevant for the future. Countries may be able to effectively utilise the period when cases are low to design their institutional, medical, economic, and social plans.
Country should also be able to channel political capital and will for the cause of public health as well as the importance of finding mechanisms for collaboration.
Additional information:
The talk was summarised by the National Health Security Office (NHSO), see here, and also featured in a Thai news article, see here.
The video of the webinar is available here.